Symptoms of Pulmonary Tuberculosis
-Persistent cough with blood in sputum
-Cough up thick, tenacious mucus in the morning.
-Dry, nonproductive cough.
-Cough aggravated by lying on the left side.
-Ribs appear to be uneven while breathing in deeply.
-Deep breath causes increased pain in the chest area while suffering from tuberculosis.
Common causes of gallstones:
Excess weight and obesity are common causes of gallstones (gallbladder), especially when women go through menopause; excess fat deposits around the waist cause biliary stasis and an increase in cholesterol levels, which can lead to the formation of stones or gravel in the gallbladder and eventually infection if not treated properly.
Other causes include:
too much-processed fats and salt intake; heavy drinking, hard liquor without enough water; deficiency of nutrients needed for making bile, such as vitamins A and B12.
Symptoms of gallstones:
-Chills are running down back or between shoulders blades.
-Pain starts from the left shoulder blade and spreads to the neck, chest, back, and abdomen on the same side.
-Sharp pain in ribs when breathing deeply or coughing; worse with first breath in the morning after waking up.
-Worse with eating fatty foods like meat, fried foods, ice cream, etc.; drinking alcohol; smoking cigarettes; anxiety; stress.
Gallstones are hard pebbles that form inside the gallbladder by crystallizing excess cholesterol or pigments in bile needed to digest fat properly.–Many people mistake gallstones for kidney stones because of similar symptoms, but there are some differences between them.
Kidney stones cause pain in the loin and lower abdomen on both sides of the body simultaneously, while gallstones cause left shoulder blade pain or pain on one side of the liver. Kidney stones usually dissolve naturally on their own without any treatment, so people who suffer from kidney stone attacks will feel relief within 48 hours.
-Gallstones do not disappear on their own and can lead to tend tendinous inflammation and infection if not treated properly, which is why you must see a doctor about this problem right away before it gets worse.
The reason for gallstones:
There are many reasons why gallstones form in the body, like having too much cholesterol in the liver and difficulty making bile digest fat properly, leading to excess cholesterol or pigments that crystallize and form stones. People who drink excessive alcohol are also more likely to develop gallstones because this increases the bloodstream’s fats and harmful cholesterol levels.
-Excessive intake of oily fish like salmon, mackerel, etc., lack of physical exercise or workout; high consumption of carbohydrates can also cause gallstones.–A sedentary lifestyle is one of the leading causes for obesity these days, so you must do some relief yourself by exercising at least 30 minutes every day or walking around your house if you can’t afford gym membership yet.
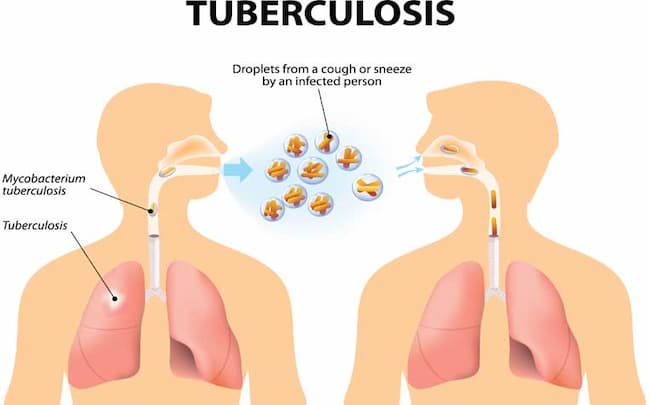
Pulmonary tuberculosis causes:
1. it is caused by mycobacterium tuberculosis, bacillus Calmette-Guerin (BCG) vaccination is used to prevent tuberculous meningitis and miliary tuberculosis in young children
2. it causes inflammation of the lungs
3. bacteria most commonly reach the lungs via the bloodstream from another site of infection such as the genitourinary tract or gastrointestinal tract/pulmonary TB also occurs after spread from nearby tissues, even years after initial infection.
4. Symptoms include a prolonged cough, blood-tinged sputum, fever, chills, night sweats, weight loss, and fatigue.
5. Diagnosis can be confirmed with a chest X-ray finding typical of pulmonary TB or a tuberculin skin test.
6. Treatment is with several antibiotics such as rifampicin, isoniazid, pyrazinamide, and ethambutol for two months, followed by isoniazid and rifampicin for at least four more months.
7. Tuberculosis has an extensive range of symptoms depending on the site affected: it can involve any organ system in the body but generally involves the lungs (respiratory symptoms), kidneys (genitourinary symptoms), or larynx/pleura/peritoneum/mesentery (visceral symptoms).
8. It is among the top ten causes of death worldwide.
What is the first sign of tuberculosis:
1. Cough, which is often dry and may persist for weeks or months
2. Weight loss, exhaustion, and malaise
3. Fever/night sweats
4. Weakness and fatigue
5. Anorexia, nausea, and vomiting
6. Headache/meningism
7. Lymphadenopathy (enlargement of the lymph nodes)
8. Hepatosplenomegaly (enlarged liver and spleen)
9. Arthralgia (joint pain), arthritis (often in weight-bearing joints such as knees and hips).
10. Pleural effusion (lung infection)
pulmonary tuberculosis diagnosis:
1. Physical examination
2. Chest X-ray
3. Pulmonary function tests (PFT)
4. Sputum smear and culture for mycobacteria in tuberculosis
5. AFB PHLMI TB test in diagnosing pulmonary TB in HHC centers/private sector clinics in India, when conventional methods are inconclusive or unavailable.
7. TST is done to assess the degree of immune responsiveness against M .tuberculosis antigens, both quantitatively and qualitatively, using commercially available intradermal assays for TST reagents, which are not only time-efficient also cost-effective as well as user friendly when compared to the Mantoux technique for TB screening.
8. Immunological diagnostic tests are only recommended to diagnose latent TB infection in adults who can return to their doctor within two weeks for a final evaluation if the test results are positive.
9. Goals of therapy include cure, defined as being free of all disease after completion of treatment; preventing or curing sequelae, usually by reducing the level of active disease before starting therapy; limiting progression and complications; improving quality of life; extending survival; and decreasing transmission.
10. Analysis: The results showed that the TST positivity rate was 31% with an increased proportion (63%) tested with TST+ve in recent years and suggestive evidence (P < 0.05) that several persons screened are adequately responsive to rising prevalence rates observed in India.
11. Self-reported history of having tuberculosis was reported for 1,987 subjects, all of whom underwent PFT and were found to have restrictive lung function impairment. The prevalence of latent TB infection in this population was 47%.
Tuberculosis prevention:
1. ß-lac t is recommended for health care workers who are repeatedly exposed to patients with infectious TB disease
2. Isoniazid chemopreventive therapy may be given to individuals at risk of it due to living in areas where the prevalence of HIV infection is high (e.g., sub-Saharan Africa)
3. Bacillus Calmette Guerin vaccine ( BCG ): Treatment with bacilli Calmette Guerin (BCG), a live attenuated vaccine derived from an avirulent strain of M .tuberculosis, has been used successfully in high incidence countries such as the Russian Federation and China, but it has proved disappointing in most other countries vaccine efficacy estimates vary between 15 and 86%
4. Tuberculin skin testing (TST) is widely used in many settings. Still, it has several limitations, such as the necessity for periodic testing, the need to obtain intradermal results to make a diagnosis, and its lack of specificity in persons infected with other mycobacteria.
5. STI control: at least 50% of incident cases in some populations occur among people who are already infected with another sexually transmitted pathogen (e.g., N gonorrhea tr, Cachomatis ). Therefore screening tests for curable diseases should be offered to all individuals attending STD clinics. Further, condom distribution programs have been demonstrated to reduce tuberculosis incidence by 80% or more when implemented on a wide scale.
Latent tuberculosis diagnosis:
1. The new algorithm developed by the American Thoracic Society/CDC/Infectious Diseases Society of Ameri can (ATS/IDSA) recommends, in addition to chest X-rays, either two tuberculin skin tests (TST) or interferon-gamma release assay (igra).
2. Sputum smear microscopy remains an essential tool for the initial evaluation of suspected TB cases either in hospital-based facilities, public health departments, and TST positive laboratory units /hospitals with proper infrastructure; it should be performed before administering isoniazid preventive therapy (IPT) to determine if there are any pulmonary TB patients whose bacterial load may be too great for successful treatment with short-course chemotherapy.
3. The most common sites of extrapulmonary tuberculosis are lymph nodes, kidneys, bones, joints, and the central nervous system (CNS). Involvement of the CNS is secondary to hematogenous spread or direct spread from either a primary or secondary focus elsewhere in the body.
4. Treatment for latent TB infection is based on an individual’s risk factors for having a lab. These include age older than 35 years, HIV-positivity, residence in a community with a high prevalence rate of tuberculosis, history of positive TST result within the past two years, or chest radiograph findings consistent with active TB disease
5. The only currently available vaccine that has been effective against TB is the Bacille Calmette Guerin vaccine (BCG). The only available prophylactic therapy is the treatment for latent TB infection.
6. Isoniazid chemopreventive therapy may be given to individuals at risk of it due to living in areas where the prevalence of HIV infection is high (e.g., sub-Saharan Africa)
7. Chest X-ray: should be considered in all suspected tuberculosis cases, but it is specifically indicated when extrapulmonary tuberculosis is suspected or when clinical findings are atypical. It has no role in diagnosing pulmonary TB, particularly in patients who have completed a course of chemotherapy
8. Sputum collection: if sputum production can be elicited, it should be collected for acid-fast bacilli smear microscopy, quantitative cultures, or both. Sputum must be maintained on the ice at all times.
9. Treatment of TB takes six to nine months and is prolonged because of the slow growth of M tuberculosis in human hosts, although the active disease may resolve rapidly during the first two weeks of treatment.
Once a patient has begun chemotherapy, chest radiography is repeated three months after starting treatment to detect active disease. If signs of active infection are still present, treatment continues for another three months; if no evidence of active disease remains, therapy can stop.