What is the Treatment of An Electrocardiogram?
The treatment for the EP is by electrical cardioversion. Electrical cardioversion consists of applying a brief, high-energy electric shock to the chest to depolarize all heart muscle cells at the same time.
Using this technique, it is possible to restore normal sinus rhythm within seconds in about 90% of patients with atrial flutter and 70-80% in patients with AV nodal reentrant tachycardia (AVNRT).
Electrical cardioversion may be performed either externally or internally. External cardioversion involves applying electrodes to the person’s chest and delivering a shock from outside. In contrast, internal cardioversion consists in passing a catheter into one or both of the heart’s chambers and applying the shock from within. Usually, internal cardioversion is preferred with these arrhythmias because it carries less risk of complications than external cardioversion.
The primary purpose of this treatment is to achieve sinus rhythm quickly without any cardiovascular side effects or difficulties.
Electrical cardioversion requires two people to place the electrode pads on the patient’s chest and deliver the shock while another person waits by with an oxygen supply.
Before delivery of an electrical shock, intravenous sedation may be used. This is so that when electrical cardioversion occurs, there will not be any physical resistance that may cause harm to both parties involved in the procedure.
The patient will be awake during the procedure and feel a sudden jolt when the shock is delivered. After electrical cardioversion, the patient may feel lightheaded, dizzy, or weak, and they must be monitored closely until these symptoms have passed.
Complications associated with electrical cardioversion are rare but can include:
Arrhythmias can occur in up to 10% of patients following electrical cardioversion and can persist for some time afterward.
Myocardial infarction (heart attack) is very rare ( occurring in less than 0.1% of cases) but can happen if there is underlying coronary artery disease.
Pulmonary embolism (PE) is an uncommon complication (occurring in less than 0.1% of cases).
For the same reason, electrocardiogram treatment includes protection against external shocks to the patient’s heart.
The entire procedure lasts for up to 30 seconds which is longer than many other systems, but it does not cause any pain or discomfort. It takes about 10 minutes to complete and requires no recovery time before returning home.
It can be performed on conscious and unconscious patients awake during the whole procedure. A defibrillator would monitor the patient’s heart rate, so there is no risk of human error occurring during the process.
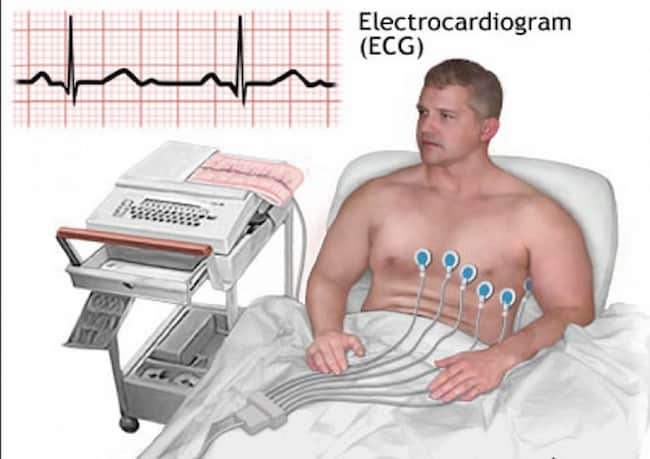
ECG procedure:
The patient is initially asked to rest in the supine position for about five minutes. Then they are made to sit upright and remain still while electrodes (sticky pads) with wires are attached at specific locations on their chest, arms, and legs.
These sticky pads act as recording electrodes for picking up electrical signals from the heart muscles. They correspondingly get transmitted through these wires to an ECG machine, which visibly displays in terms of waves.
The recorded tracings represent the pattern of electrical impulses originating within the heart due to actual events like contraction of each heart chamber etc., that occur during every cardiac cycle.
A typical ECG tracing consists of a sequence of vertical or perpendicular lines arranged one after another in a definite pattern known as leads, i.e., II, III, and AFV (atrial flutter) in the frontal plane, and I, II, and -aVF in the horizontal plane.
Six leads are labeled as I, too -VI in both planes. The various waves visible in an ECG tracing correspond to electrical forces generated by specific events occurring within the heart muscles.
For instance, a P wave represents atrial depolarization; QRS complex is due to ventricular depolarization; T wave is caused by ventricular repolarization; while U wave relates to slow ventricular repolarization between beats, i.e., during the relaxation phase of heart muscle cells.
How is an ECG performed on a woman:
An ECG for a woman differs from a man’s in the placement and number of electrodes used. The female chest is flatter than the male’s, so it’s easier to place electrodes during an ECG test. A 12-lead ECG can be performed on women if necessary, but, traditionally, only six leads are performed: one information on each arm and leg and three “leads” across the chest (V1, V2, and V3).
The V4 “lead” is not placed as this would cover two heartbeats of relevant data at rest, thus rendering them useless. During exercise, more leads may be required.
Electrodes for women:
Sometimes extra electrodes (sticky patches) are placed on the breasts to get a clearer tracing (this is more common in older women and those who have had a mastectomy). However, any breast tissue resting on the electrode will create an artifact (distortion) on the ECG.
The placement of electrodes is slightly different for pregnant women. The electrodes are placed on the woman’s abdomen, below the navel, and to the left of the belly button. This is so that the electrical signals from the baby’s heart can be recorded.
There are also specific instructions for taking an ECG during labor. First, the electrodes are placed on the mother’s back, just below her shoulder blades. This allows the doctor to see how the baby’s heart responds during contractions.
What information does ECG give about a person?
An ECG gives a doctor information about the heart’s rhythm, the size of the chambers, and how well the valves are working. It can also show a previous heart attack, heart failure, or electrolyte abnormalities.
The most common use for an ECG is to determine if someone has a heart attack. The test can show damage to the heart muscle and help doctors decide whether or not to give a patient drugs like aspirin or thrombolytics (medications that break up blood clots).
An ECG can also help diagnose other problems with the heart, such as arrhythmias (abnormal heart rhythms) and cardiomyopathies (diseases of the heart muscle). However, it is essential to remember that an ECG is only one piece of the puzzle when diagnosing a heart problem.
Diagnostic use:
An ECG test can be used for several diagnostic purposes. A routine ECG in “standard” lead positions provides cardiac anatomy, activity, electrical conduction, and muscle mass. It may indicate acute coronary occlusion (a blood clot blocking blood flow) or an electrolyte disorder.
An electrocardiogram is also helpful in detecting many conditions involving damage to the myocardium (heart muscle). These include coronary artery disease, hypertrophic cardiomyopathy, pericarditis, pulmonary embolism or infarction, restrictive cardiomyopathies, and valvular heart disease.
It helps diagnose some specific conditions, including pericarditis (inflammation of the membrane surrounding the heart), pulmonary embolism (a blockage in an artery to the lungs), or infarction (localized death of tissue).
It can be used to help determine the cause of chest pain, shortness of breath, fainting spells, or palpitations. For instance, it can distinguish between these symptoms due to problems with the lungs and problems with the heart.
An ECG may also detect many more abnormalities not listed here. A report generated by a computer after an ECG test will document any abnormal findings encountered during its analysis; this information will be discussed with patients by physicians.
The use of 12-lead ECGs has increased the ability to diagnose conditions that originate from outside of the heart. For example, an ECG may help identify abnormalities in the brain’s electrical activity, such as a seizure. It is even used occasionally to diagnose problems with muscles, such as myopathy or polymyositis.
An ECG should not diagnose mental health disorders such as panic attacks or anxiety disorders. Electrocardiograms are relatively inexpensive, noninvasive tests widely available in most hospitals and clinics.
They provide valuable diagnostic information for patients with chest pain, shortness of breath, and other symptoms that may indicate a problem with the heart. Physicians often order them routinely for patients who complain of these symptoms, especially over age 40. This is to detect coronary artery disease or a heart attack in its early stages.
An ECG can also be beneficial in diagnosing many other problems. For example, it may indicate whether a person is having a stroke by showing an interruption in blood flow to the brain. An electrocardiogram may show irregularities in rhythmic contractions of the heart muscle (arrhythmias).
It also helps determine if someone has high potassium, magnesium, and calcium levels by measuring how long it takes for each ion to cross the cell membrane barrier and leave the cells that produce the electrical impulses that initiate contraction.